“For me, a child is a blessing,” says Abigail Hendricks, who benefited from a brand new drug trial for preeclampsia. Right here she is along with her nearly 9-month-old, Hayden
Tommy Trenchard for NPR
disguise caption
toggle caption
Tommy Trenchard for NPR
It was the autumn of 2024 when Abigail Hendricks discovered she was pregnant along with her fifth baby. She was glowing with pleasure.
“For me, a child is a blessing,” says Hendricks. “They’re cute. They’re treasured. And they’re a present from God.”
However Hendricks, who was 33 on the time and dwelling in Cape City, South Africa, would later be taught that her rising child was additionally a grave well being threat to her. Hendricks already had hypertension. Quickly, the complications started. Once in a while, her imaginative and prescient would blur. Then protein began exhibiting up in her urine.
“I stored on preventing,” she remembers. “I did go to church. I pray within the morning. I pray at night time for my child to be secure and for me to be secure.”
Her medical doctors put her on a distinct blood strain remedy and advised her to relaxation. By this time, all of Hendricks’ appointments had shifted to Tygerberg hospital, a facility in Cape City geared up to deal with extra advanced instances.
However a month earlier than she was because of give start, she was shedding blood strain management. A traditional studying is 120 over 80, however hers climbed to 163 over 101.
Hendricks had developed preeclampsia, a doubtlessly deadly complication of being pregnant involving injury to the blood vessels and excessive quantities of fluid loss. It will possibly result in harmful swelling of the lungs, mind, and coronary heart and big hemorrhaging.
“They advised me I can have a seizure as a result of the blood strain is simply too excessive,” she says. “It made me really feel scared and fearful. Like, what will occur now?” (Eclampsia refers back to the seizures that happen in pregnant girls with preeclampsia.)
The medical staff believed Hendricks’ life was at risk — and so was her child’s.
An anxious starting

Cathy Cluver, professor of obstetrics and gynecology on the College of Stellenbosch (proper), embraces a pregnant mom at Tygerberg Hospital in Cape City. “Your child’s very excited to return and meet you,” she tells her. Cluver, leads a analysis staff conducting a trial for a brand new drug to deal with preeclampsia, a doubtlessly harmful situation throughout being pregnant.
Tommy Trenchard for NPR
disguise caption
toggle caption
Tommy Trenchard for NPR
On a latest morning, Cathy Cluver glides by means of the bustling maternity ward of Tygerberg Hospital. Provide carts are wheeled down the hallway. Nurses and medical doctors transfer between their many sufferers. A new child child’s first cry pierces the air. Cluver is a professor of obstetrics and gynecology at close by Stellenbosch College, and she or he’s been looking for a therapy for preeclampsia for a decade.
“We do about eight to 9,000 deliveries right here a yr of solely high-risk girls,” explains Cluver, together with these with preeclampsia who do their greatest to delay supply. It is essential for a child to remain contained in the womb so long as potential however this may jeopardize the well being of the mom.
Cluver factors to a room containing moms with preeclampsia. “You may see they are not trying properly,” she says. “Their toes and their legs are swollen, and their palms are swollen. These mums are placing their very own lives in danger for the sake of the infant.”
Preeclampsia happens when the placenta sends out a sort of molecular misery name that it is not getting sufficient oxygen. “It is saying, ‘I want extra blood provide, so I will push the blood strain up,'” says Cluver, who had preeclampsia herself when she was pregnant along with her first baby.
Standard drugs to deal with hypertension are dangerous as a result of although they may decrease the mom’s blood strain, they could additionally scale back blood movement to the infant — proper when the placenta is demanding extra oxygen.
“It actually is among the most severe issues of being pregnant,” says Cluver, making it one of many main causes of maternal mortality worldwide — with no less than 42,000 maternal deaths annually.
Cluver has been looking for a therapy that lowers blood strain and heals the broken blood vessels to assist each mom and child. Then, about two years in the past, she bought an e mail from DiaMedica Therapeutics, a U.S.-based pharmaceutical firm.
They have been testing a drug for sure varieties of stroke known as DM199 that functioned in a means they thought may also work for preeclampsia. Cluver was skeptical at first, however on nearer inspection, she and her colleagues thought perhaps it was price making an attempt out. “It may doubtlessly work as a result of it is ticking all of the packing containers of what we might need,” she says.
In order that they started a trial on the hospital for moms with dangerously hypertension and who have been scheduled to ship their infants early.

Jacqui Thake, a analysis nurse at Stellenbosch College who’s overseeing the drug trial, measures the blood strain of one of many sufferers on the hospital.
Tommy Trenchard for NPR
disguise caption
toggle caption
Tommy Trenchard for NPR
“I used to be so nervous that first day,” says Cluver. “We began the infusion and also you by no means fairly know what is going on to occur.”
The staff enrolled small teams of girls with every group receiving a barely larger quantity of the drug. Fifteen sufferers in, there was no signal that it was having any impact.
“I believed, ‘this drug is just not actual,'” says Jacqui Thake, a analysis nurse at Stellenbosch College who’s overseeing the trial. “There was actually no distinction within the blood strain — perhaps barely right here and there however nothing main.”
Fortunate quantity 16
When the sixteenth affected person obtained the following highest dose, nonetheless, “we actually simply opened up this IV infusion after which her blood strain stabilized,” remembers Cluver. “We abruptly noticed these sky-high blood pressures coming down and we have been like, ‘We do not consider this. That is not possible!'”
“That is really when the actual pleasure began,” says Thake. “Like leaping up and down. I [sent] a gazillion emojis celebrating the blood strain taking place.”
And it stayed down. The identical was true for subsequent sufferers with the identical or incrementally larger doses.
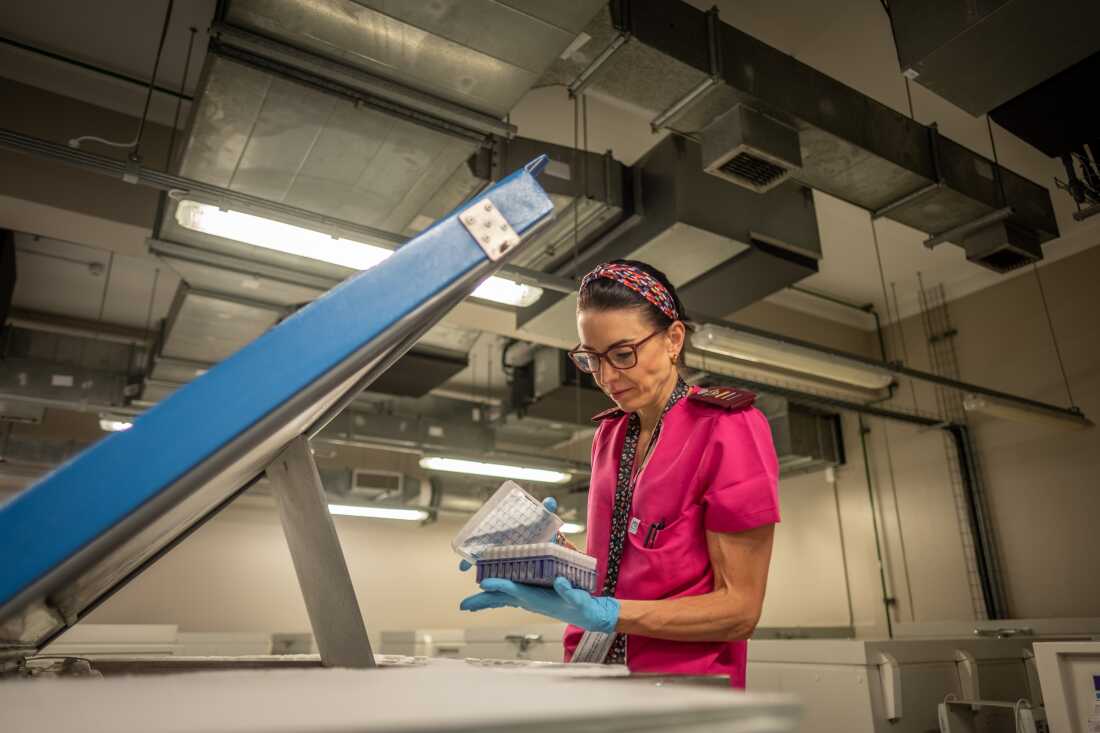
The drug trial requires the common sampling of the blood of contributors. Right here, analysis nurse Jacqui Thake pulls out a handful of these samples from one of many -80°F freezers.
Tommy Trenchard for NPR
disguise caption
toggle caption
Tommy Trenchard for NPR
“The drug stabilizes the liner of the blood vessels so it makes the blood vessels happier,” says Cluver.
Assessments present the drug would not seem to cross into the placenta or the breastmilk both, which implies it is probably not reaching the infant.
Cluver and her colleagues are hopeful that this may be the primary pharmaceutical therapy for preeclampsia.
“It will imply a wholesome mother and a wholesome child,” says Thake, who talks about what it may be wish to lose a mom or baby. “It will imply much less damaged properties and presumably a greater life for the little ones rising up. That is what it will imply to me — a mother and a child rising up with love.”
Nonetheless, she says there’s extra to find out about how the drug works and whether or not it might maintain moms pregnant for longer.

This frozen vial accommodates DM199, a brand new experimental drug that researchers hope stands out as the first pharmaceutical remedy for preeclampsia.
Tommy Trenchard for NPR
disguise caption
toggle caption
Tommy Trenchard for NPR
Corneila Graves is the medical director of Tennessee Maternal Fetal Medication, a facility the place she says as much as 10% of pregnant girls have preeclampsia.
“It is a small examine — it has nice potential however we want an even bigger knowledge set on a broader inhabitants,” says Graves, who is just not concerned within the trial.
“However what is absolutely promising about this specific examine is that it additionally will increase placental blood movement,” she provides. That’s, this new drug lowers the mom’s blood strain whereas additionally bettering blood movement to the womb at a time when the infant seems to wish it.
Kara Rood, a maternal fetal medication doctor on the Ohio State College who is not contributing to the trial, feels equally inspired by the early outcomes. However she’s desirous to see how the drug impacts girls earlier of their pregnancies and never within the pressing moments proper earlier than their supply.
“I believe the actual check can be whether or not this remedy can safely extend the being pregnant to lower these dangers and in the end enhance neonatal outcomes,” says Rood.

Analysis nurse Jacqui Thake walks alongside Abigail Hendricks and her child boy. When Hendricks turned affected person quantity 24 within the drug trial, the 2 girls fashioned a particular bond.
disguise caption
toggle caption
As for Abigail Hendricks, she was affected person quantity 24 within the trial at Tygerberg hospital. Her child son is nearly 9 months now. “Hayden is a candy little boy. He is very playful.”
Again when her blood strain stored going up final yr a number of weeks earlier than her due date, she enrolled within the trial and obtained the brand new drug simply earlier than the medical staff induced her. Hendricks’ blood strain slowly dropped.
After which, “he was delivered screaming,” she says. “Once I held my child for the primary time, I cried. I had a lot pleasure in my coronary heart to know that he’s alright. And I used to be alright.”
This story was supported by a grant from the Pulitzer Middle.